Just Launched: Instantly Spot Gaps in Medical Reporting
In life and disability underwriting, one of the most time-consuming and error-prone steps is verifying an applicant’s self-reported information.
Why? Because applications are long and detailed, and even when applicants are trying to be honest, omissions, intentional or not, are common. This is a growing concern across the industry, a recent Munich Re’s survey identified applicant misrepresentation as the most rapidly increasing form of fraud.
Sixfold’s Discrepancy Scan capability was built to address exactly this issue. Sixfold’s AI is now able to automatically flag mismatches between what applicants report and what’s found in their medical records, giving underwriters a faster, more standardized way to catch inconsistencies before they become costly.
When risk is hiding in the records

When someone applies for individual life or disability coverage, they complete a health questionnaire, like Part II, eMed, or a Med Supplement, disclosing conditions, medications, and history. From there, the underwriter kicks off verification: ordering APS reports, Rx histories, labs, and other third-party records.
As these often hundreds of pages of documents arrive, the underwriter is essentially playing detective — comparing what the applicant said to what the medical records reveal. Did the applicant disclose all relevant conditions? Are they taking medications they didn’t mention? Is there a difference in diagnoses or treatment history?
Underwriters dedicate significant time to identifying discrepancies because they are critical. A person's prescription history can reveal underlying health issues, sometimes even before a formal diagnosis is made. For example, a prescription for a weight-loss medication might indicate an associated morbidity.
Any inconsistency could signal fraud or simply an oversight. Either way, it matters.
See below for a quick product walkthrough with Noah Grosshandler, Product Manager at Sixfold.
The feature is currently focused on medications, but that’s just the beginning. We're planning to expand this capability to detect discrepancies across pre-existing conditions, procedures, family history, and lifestyle factors—always guided by what’s material to each insurer.
Minutes vs. hours of detective work
Sixfold’s new capability eliminates a critical bottleneck in underwriting. The traditional approach of manually reviewing hundreds of pages to spot inconsistencies is both time-intensive and susceptible to oversight.
The Discrepancy Scan changes that completely, surfacing critical discrepancies automatically instead. The result is a more efficient process where underwriters can confidently assess risk based on complete information, without the administrative burden of document comparison.
“Sixfold goes beyond summarizing medical histories, we spotlight the contradictions that can change a morbidity assessment. By drawing connections across medical records, we emphasize the most crucial facts for investigation.
This approach transforms hours of detective work into minutes, providing underwriters with confidence and efficiency in their decision-making processes.”
— Lana Jovanovic, Head of Product @ Sixfold
Get the full story upfront
Accuracy is everything in life and disability underwriting. With Sixfold’s automatic discrepancy detection, underwriters are able to get to a more accurate underwriting decision by:
- Catching omissions and inconsistencies at the beginning of the review cycle
- Reducing misclassification of risk due to overlooked or conflicting information
- Detecting potential fraud patterns before they result in costly claims
- Maintaining consistency and transparency when cases move between underwriters
How the feature works
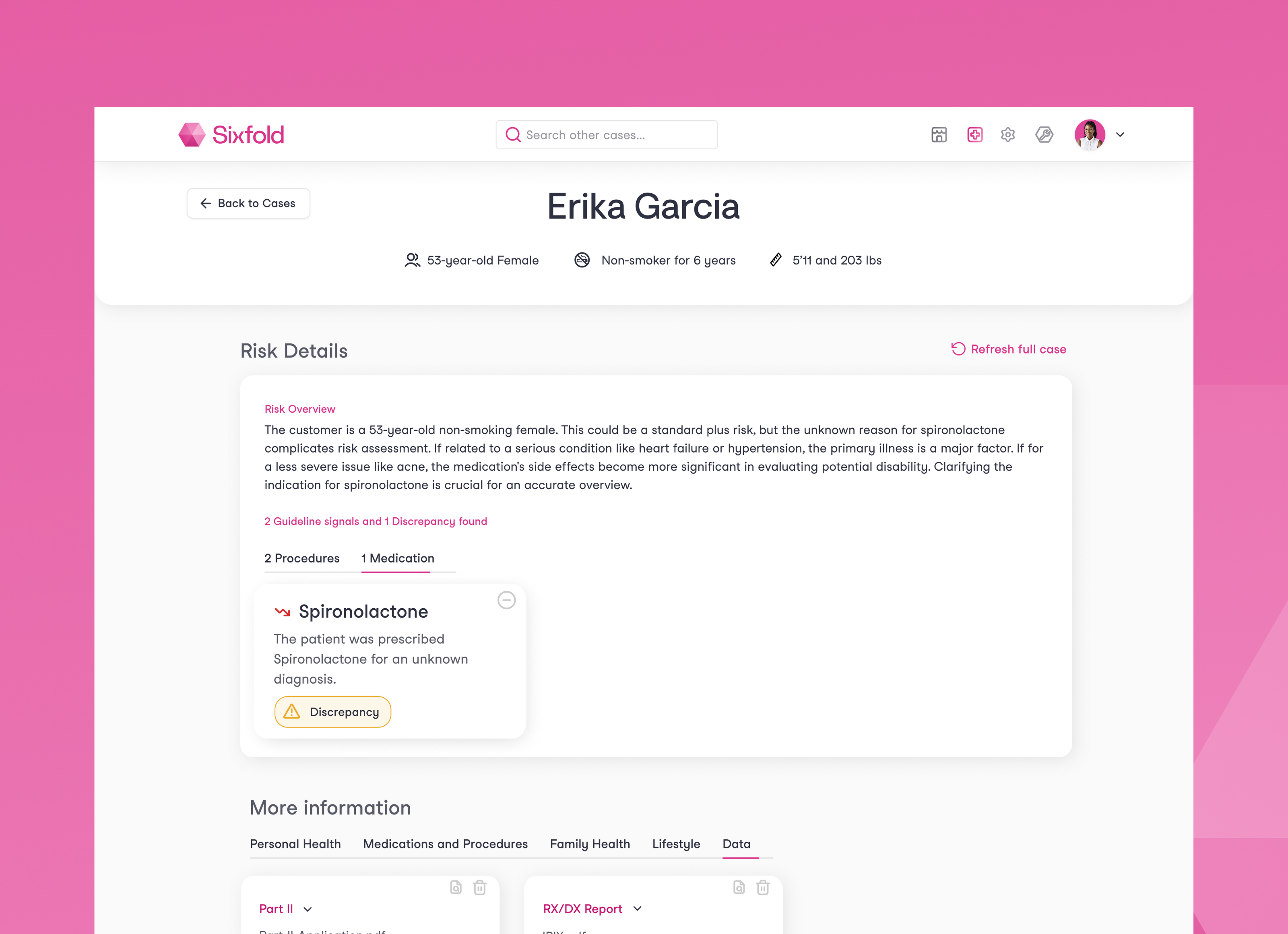
The Discrepancy Scan automatically compares the self-reported application data against the supporting medical documents and flags any mismatches related to material facts.
Prescriptions are often a leading indicator of an underlying diagnosis, one that could directly impact insurability or rating decisions. But not every medication matters the same way, and what’s considered “material” varies from carrier to carrier.
By securely ingesting each carrier’s unique underwriting guidelines, Sixfold identifies which medications are truly relevant in each context, connecting the dots between prescriptions, diagnoses, and underwriting impact.
Here’s how the feature works in practice:
1. Medical Document Review
Sixfold’s AI reviews both the submitted application and any supporting documents uploaded (APS, MIB, Rx histories, etc.) for medical data relevant for risk assessment.
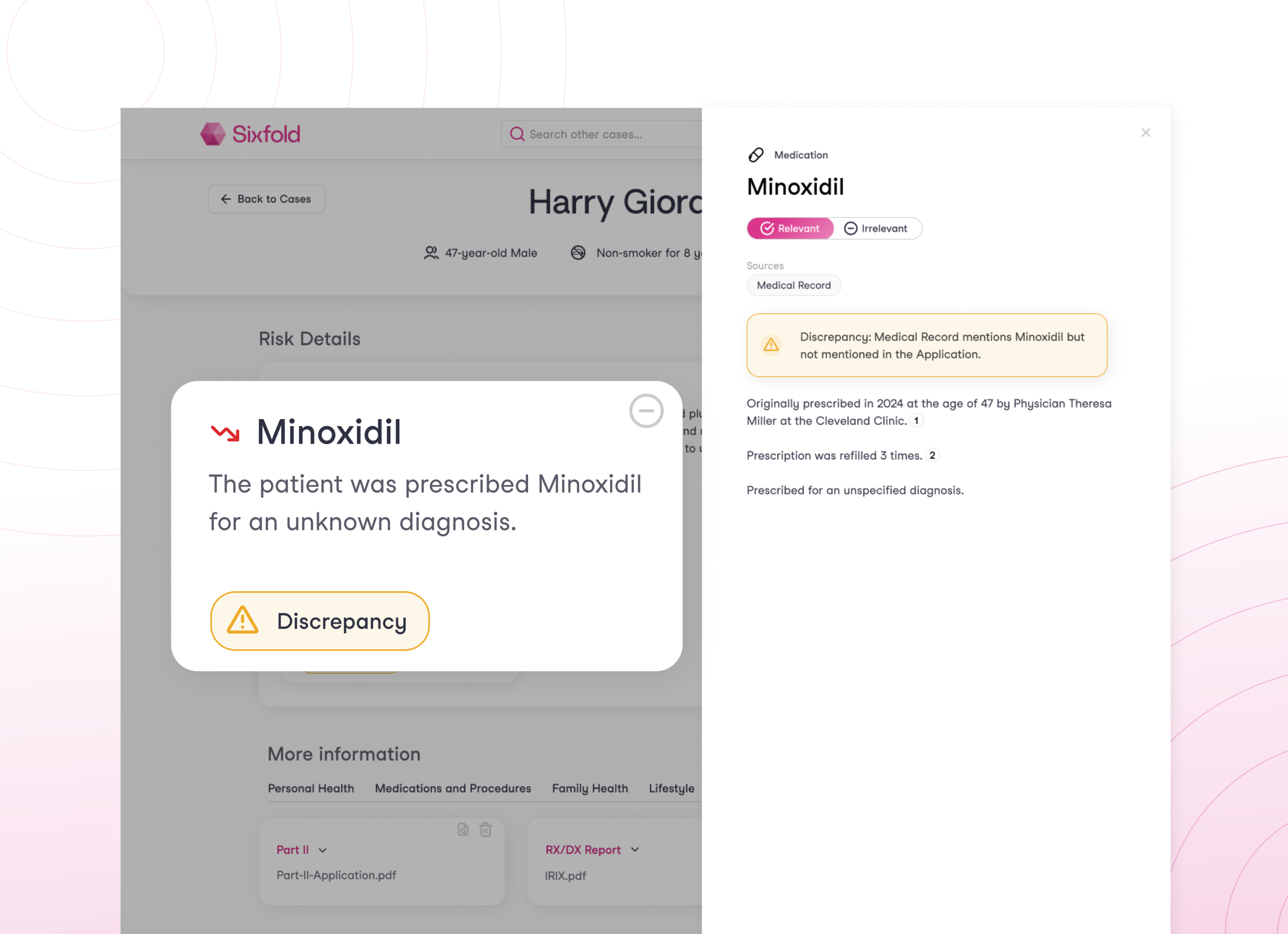
2. Discrepancy Detection
Sixfold then compares the findings in the medical documentation to what the applicant reported. If a medication appears in the documents but not in the application, it’s flagged as a discrepancy.
3. Discrepancy Alert
Within the underwriter's dashboard, discrepancies appear clearly labeled with clear icons. Clicking into a card brings up the relevant context e.g., “Blood thinner mentioned in the medical report, not disclosed by the applicant.”
4. Clear Next Steps
Underwriters can use this insight to request clarification from the applicant or additional documentation from providers.
5. Always-Current Monitoring
Because documents arrive asynchronously, the system continually updates as new files are uploaded. Discrepancies are flagged dynamically based on the most current information.
Learn More
Insurtech Insights takes a closer look at the Discrepancy Scan
Interested in a hands-on demo? Reach out for a Sixfold walkthrough

